When it comes to rural living, Vermont wears the crown. According to the 2020 Census, 65% of Vermonters live in rural areas, making it the most rural state in the country. But with that title comes a challenge that’s harder to see at first glance: the quiet disappearance of independent doctors — and what that means for the future of care in Vermont’s small towns.
A new report from the Physicians Advocacy Institute and Avalere Health spells it out:
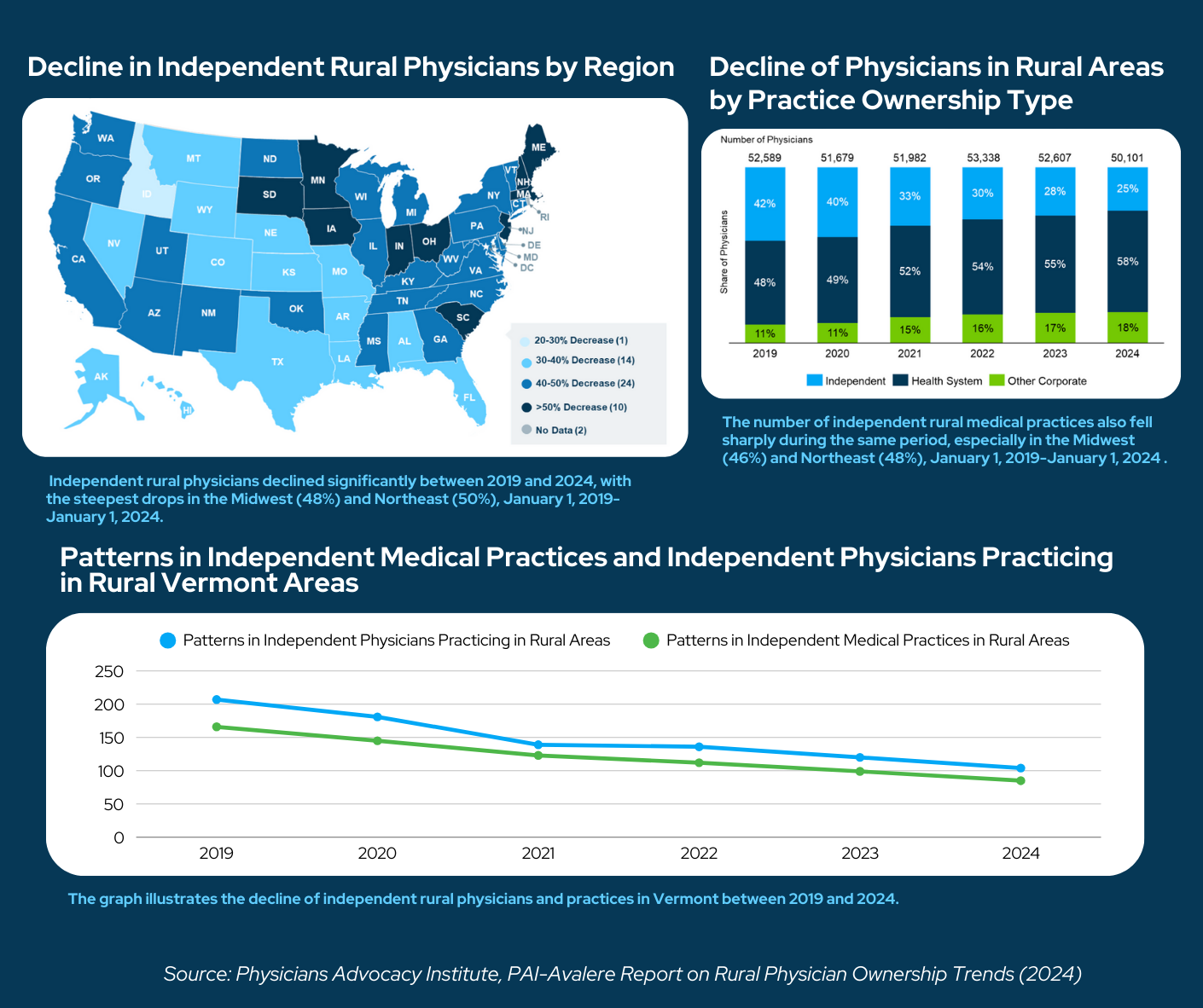
- Between 2019 and 2024, rural America lost nearly 2,500 independent physicians.
- About 3,300 rural medical practices shut down.
- Corporate ownership of rural medical practices nearly doubled.
The Northeast — Vermont included — was hit especially hard. Some states saw more than a 50% decline in independent rural physicians. In a state already struggling with thin primary care networks, the loss of independent providers means longer waits, higher costs, and fewer doctors who live in — and understand — the communities they serve.
What’s at Stake for Vermont?
When small practices close their doors or get swallowed by large health systems, it doesn’t just change who owns the practice. It changes how healthcare happens. In a rural place like Vermont, losing local, independent doctors means:
- Longer wait times and fewer local options.
- Higher healthcare costs
- A loss of personal connection, where healthcare becomes more corporate and less community-centered.
And Vermont’s rural healthcare system was already fragile. Data from the Vermont Department of Health shows some rural counties struggle with critically low primary care provider-to-population ratios (VDH, 2024). Meanwhile, recruiting new doctors isn’t easy. A 2023 pilot study, conducted by medical students from the UVM Larner College of Medicine and healthy aging advocacy group Windham Aging, found that in rural Vermont what mattered most to healthcare workers wasn’t just the paycheck — it was things like affordable housing, strong community ties, and real experiences practicing rural medicine during training (Cureus, 2023).
And as a recent article from Boston University highlighted, for many doctors, rural medicine offers rich rewards — deeper relationships with patients, greater autonomy, and a stronger sense of purpose (BU Today, 2024). The catch? Doctors need to experience that rural life firsthand before deciding to stay.
How The Vermont AHEC Network is Building the Next Generation
This is where the Vermont Area Health Education Centers (VT AHEC) Network steps in — not just plugging holes, but building a better pipeline for rural healthcare.
Here’s how they’re getting it done:
- Sparking interest early: The VT AHEC Network has introduced over 5,595 students — from middle school to college — to careers in health and medicine just in the last year (Vermont AHEC Annual Report, 2024).
- Training in the field: Programs like AHEC Scholars are embedding medical students directly into rural clinics and hospitals. In 2024, they supported 325 future providers who are now getting firsthand experience working in Vermont communities.
- Tackling medical debt: Medical school debt is one of the biggest barriers for rural healthcare recruitment. Vermont AHEC helped administer more than $4 million through the Educational Loan Repayment Program — rewarding providers who commit to practicing in Vermont’s underserved areas.
- Placing physicians where they’re needed most: Through partnerships and support programs, VT AHEC helped place eight new physicians into rural Vermont communities last year alone — with more on the way.
It’s not just about filling jobs. It’s about redefining rural medicine as a calling — one grounded in community, purpose, and real impact.
Where We Go from Here
The trends are real. The risks are high. But so is Vermont’s commitment. In fact, it’s quietly leading a different kind of rural healthcare revolution — one rooted not just in incentives, but in belonging. In relationships. In resilience.
By focusing on community connection, early exposure, and supporting healthcare workers beyond the paycheck, Vermont is doing more than reacting to a crisis — it’s building a new, more resilient rural healthcare system.
In the words of one rural doctor featured by BU Today:
“When you practice in a small town, you don’t just treat patients — you become part of their lives.”
And that’s exactly what’s at stake — and what VT AHEC and so many others are working hard to protect.
Vermont’s rural character is one of its greatest strengths. But it also means that keeping healthcare local, affordable, and personal takes real work and real investment.
Thanks to efforts like those from the VT AHEC Network, the future is still being written — by the next generation of healthcare workers who believe in rural Vermont just as much as the rest of us do.
Sources:
